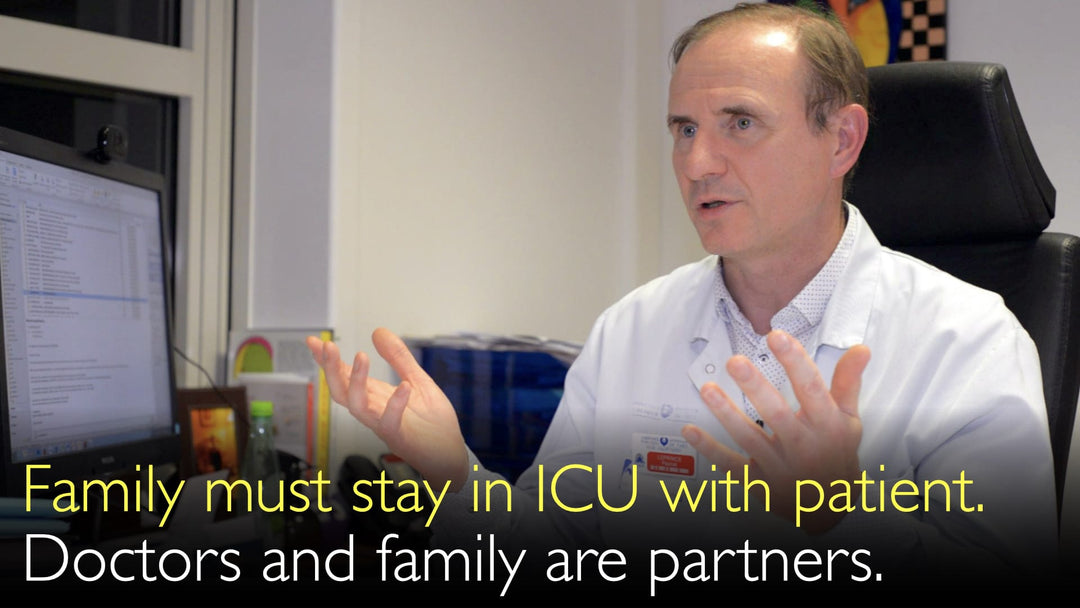
מומחה מוביל בכירורגיית לב ובהשתלות, ד"ר פסקל לפרינס, MD, מסביר את החשיבות הקריטית של נוכחות המשפחה ביחידה לטיפול נמרץ. הוא מפרט כיצד בני המשפחה מספקים תמיכה פסיכולוגית חיונית ויכולים לשתף פעולה כשותפים מרכזיים בטיפול בחולה על ידי זיהוי מוקדם של בעיות רפואיות. ד"ר לפרינס תומך בגישה טיפולית שיתופית שבה רופאים, אחיות ומשפחת החולה פועלים יחד להשגת התוצאות הטובות ביותר, במיוחד כאשר החולה אינו יכול להשתתף בטיפול בעצמו.
נוכחות משפחה ביחידה לטיפול נמרץ: רכיב קריטי בטיפול ובבטיחות החולה
קפיצה לפרק
- יתרונות נוכחות משפחה בטיפול נמרץ
- תמיכה נפשית בחולה
- גילוי מוקדם של בעיות על ידי המשפחה
- השפעת יחסי אחיות-חולים
- מודל הרפואה השיתופית
- שיתוף פעולה בצוות הרפואי
- תמלול מלא
יתרונות נוכחות משפחה בטיפול נמרץ
ד"ר פסקל לפרינס, MD, מדגיש כי מתן אפשרות לבני משפחה להישאר ואף ללון בחדר הטיפול הנמרץ מספק יתרונות עצומים. נוהג זה, הנתמך גם על ידי מנתחים מובילים נוספים כמו פרופ' לורנס ה' כהן, מהווה אבן פינה בטיפול מודרני הממוקד בחולה. היתרונות חורגים מעבר לנוחות בלבד, ומציעים שיפורים קליניים ובטיחותיים מוחשיים לחולה הקשה.
תמיכה נפשית בחולה
סיבה מרכזית לנוכחות המשפחה היא התמיכה הנפשית העמוקה שהיא מעניקה לחולה. הימצאות במצב פגיע בטיפול הנמרץ עלולה להיות מפחידה ומבודדת. פניו המוכרות של אדם אהוב מספקות נחמה, מפחיתות חרדה, ועשויות לשפר משמעותית את הרווחה הנפשית והרגשית של החולה במהלך משבר רפואי מלחיץ ביותר. תמיכה זו מהווה התערבות לא-תרופתית המשלימה טיפולים רפואיים.
גילוי מוקדם של בעיות על ידי המשפחה
ד"ר פסקל לפרינס, MD, מדגיש יתרון קריטי ופעמים רבות מוחמץ: משפחות יכולות לזהות בעיות מתפתחות לפני הצוות הקליני. מכיוון שבני משפחה ממוקדים intensely ביקיריהם, הם עשויים להבחין בשינויים עדינים במצב, בנשימה או בתגובתיות שאחות עסוקה עלולה לפספס במהלך הסיבובים. גילוי מוקדם זה מאפשר התערבות מהירה יותר, שעשויה למנוע סיבוכים ולשפר את בטיחות החולה בסביבת הטיפול הנמרץ.
השפעת יחסי אחיות-חולים
ערכה של המשפחה כזוג עיניים נוסף מועצם על ידי שינויים ברמות צוות הסיעוד. ד"ר לפרינס משווה בין מודל אחות אחת לחולה אחד הנפוץ בחלק מיחידות הטיפול הנמרץ בארה"ב לבין המציאות האירופית, שבה אחות אחת עשויה להיות אחראית על שניים או שלושה חולים קשים. בתרחישים אלה, בן המשפחה הופך לשותף indispensable במעקב, שכן האחות לא יכולה להיות נוכחת פיזית עם כל חולה בכל דקה של היום.
מודל הרפואה השיתופית
גישה זו מתיישבת באופן מושלם עם מודל "רפואת P4", שבו אחד ה-"P" מייצג "participatory" (שיתופי). ד"ר אנטון טיטוב, MD, וד"ר לפרינס מסכימים שכאשר חולה מורדם, חסר הכרה או חלש מכדי לתקשר, השתתפות המשפחה הופכת לקולו. המשפחה משתתפת באופן פעיל בתהליך הטיפול, ומבטיחה כי צרכיו והעדפותיו של החולה מיוצגים ומשולבים בתוכנית הטיפול.
שיתוף פעולה בצוות הרפואי
ד"ר פסקל לפרינס, MD, תומך בפירוק החומה המסורתית בין צוות הטיפול הקליני למשפחה. המודל האידיאלי הוא גישת עבודת צוות אמיתית שבה רופאים, אחיות ובני משפחה הם כולם שותפים מאוחדים הפועלים למען מטרה אחת - ריפוי החולה. שיתוף פעולה זה מתרחק ממערכת פטרנליסטית שבה רופאים מנווטים את הטיפול באופן חד-צדדי, ובמקום זאת יוצר מערכת אקולוגית תומכת המועילה לחולה מכל זווית.
תמלול מלא
ד"ר אנטון טיטוב, MD: אתה מאיר משהו חשוב מאוד. זו היכולת של משפחת החולה להישאר בחדר עם החולה, אפילו ברמת הטיפול הנמרץ. זה משהו שפרופ' לורנס ה' כהן הזכיר בשיחותינו לפני זמן מה. אתה אישרת זאת.
כן, כן. זה מאוד חשוב - להישאר ולישון בחדר עם קרובך. אני חושב שזה מאוד חשוב.
יש לכך שתי סיבות. הסיבה הראשונה היא העזרה הנפשית שאתה נותן לקרובך כאשר אתה נשאר באותו חדר בית חולים עם החולה. הסיבה האחרת, שעשויה להיות פחות ידועה, היא שאם אתה נשאר בחדר עם קרובך, במיוחד בטיפול נמרץ, אתה יכול להבחין בבעיות לפני שהאחיות מוצאות אותן.
מכיוון שאתה מאוד ממוקד בקרובך. בצרפת, זה שונה מאשר בארה"ב. אני זוכר שבארה"ב הייתה לנו אחות אחת לחולה אחד בטיפול נמרץ. היה קל לאחות להתבונן בחולה.
במדינות רבות, באירופה לפחות, יש לנו אחות אחת לשניים או שלושה חולים. האחות לא נמצאת עם כל חולה בכל דקה. אני חושב שדי חשוב שיהיה קרוב משפחה בחדר.
קרוב המשפחה יכול לומר שמשהו קורה לחולה ולהתריע בפני האחות. מכיוון שלפעמים חולים לא יכולים להתריע בפני האחות בעצמם. זו סיבה נוספת לכך שדי מועיל שיהיו קרובים בחדר עם החולה.
ד"ר אנטון טיטוב, MD: זה מאוד מעניין מה שאתה אומר. כי חולים דנים ברפואת P4. אחד מאותם "P" הוא "participatory" (שיתופי). זו ההשתתפות בטיפול החולה על ידי משפחת החולה.
אני מסכים שהשתתפות חשובה.
ד"ר פסקל לפרינס, MD: אין לנו יותר צוות טיפול קליני מצד אחד והמשפחה מצד שני, עם איזה קיר ביניהם. כולם מנסים לעשות את המיטב כדי שהחולה יבריא.
אנו יודעים שהשתתפות החולה בטיפול חשובה מאוד. אך אם חולה לא יכול להשתתף כי הוא ישן, או כי הוא בטיפול נמרץ, אפילו אם החולה במחלקה אך מאוד עייף כדי להתנועע, אני חושב שהשתתפות המשפחה חשובה מאוד, כמו עבודת צוות הטיפול.
זו עבודת צוות אמיתית. חולים, רופאים, כולם חלק מהצוות together, בניגוד לרופאים המכוונים את טיפול החולה באופן חד-צדדי. זה הולך לשני הכיוונים. אני מסכים שזה מאוד חשוב.